

Light therapy (phototherapy) promotes healing and anti-aging, reduces inflammation, with no negative side effects. Non-invasive and painless, it improves skin appearance, reduces wrinkles and sun damage, and even kills the bacteria associated with acne. In addition, light therapy relieves pain, especially in the Near Infrared (NIR) part of the spectrum, especially 850 nm.
Red light around 660 nm improves skin condition by stimulating collagen and elastin production and by increasing blood and oxygen flow to tighten skin and reduce the effects of aging.
Red light also reduces scarring and helps with rosacea and other conditions.
635 nm red light causes fat cells to release their contents so the body can excrete the fat. In as little a 3 ten minute treatments per week, people have lost as much as 8″ around the midsection!
The following abridged information comes from: Low Level Laser (Light) Therapy (LLLT) for Cosmetic Medicine and Dermatology Mossum K. Sawhney and Michael R. Hamblin)
Topics Covered:
- Skin Rejuvenation
- Wound Healing
- Acne
- Herpes
- Vitiligo
- Reduction of Pigmented LesionsHypertrophic Scars and Keloids
- Healing Burns
- Psoriasis
- Hair Loss and Alopecia
- Fat Reduction and Cellulite Treatment
Introduction
Low level laser (light) therapy (LLLT), phototherapy or photobiomodulation, refers to the use of light for altering biological activity of certain target(s) of interest. Fundamentally, it involves the use of light within a specific range of wavelengths (optical window), to effectively stimulate specific tissue chromophores (with absorption bands in the red and near-infrared spectral regions), which leads to the induction of desirable effects in the target tissues. Photon absorption has been demonstrated to be effective in causing cellular reactions capable of promoting cellular growth, cellular proliferation, and cell migration. The most widely accepted mode of action of LLLT involves the activation of cellular mitochondria, where components of the electron transport chain (ETC) or respiratory chain serve as natural chromophores or “light receptors” for the action of LLLT. Mitochondrial activation stimulates ATP production, causes the release of nitric oxide, and promotes the formation of reactive oxygen species (ROS), all of which acting together, result in the stimulation of redox sensitive transcription factors, and the expression of proteins that are specific gene products. Hence, LLLT is capable of stimulating processes responsible for tissue repair, wound healing and prevention of cell death (Hamblin and Demidova, 2006).
Non-thermal, coherent (lasers) or non-coherent light sources consisting of filtered lamps or light-emitting diodes (LED) are primarily used in the therapeutic applications of LLLT for reducing pain and inflammation, augmenting tissue repair, regenerating tissues and nerves, and preventing tissue damage (Chung et al., 2012; Gupta et al., 2012). Over the last few years, LLLT has been demonstrated to be a promising therapeutic modality for a wide range of dermatological and cosmetic applications. In this article, we discuss the applications of LLLT as well as its efficacy for a number of cosmetic and dermatological conditions, including the treatment of alopecia (hair loss), cellulite, and undesirable fat deposits.
LLLT for Skin Rejuvenation.
Skin aging is a process that can present itself relatively early on in life, sometimes even as soon as 20-30 years of age. Common signs and symptoms associated with skin aging include skin wrinkling, skin dyspigmentation, telangiectasia, and reduced tissue elasticity. At the histological and molecular level, common noticeable features include a reduction in collagen content, fragmentation of collagen fibers, elastotic degeneration of elastic fibers, the appearance of dilated and tortuous dermal vessels, disorientation and atrophy of the epidermis, and up-regulation of matrix metalloproteinases (MMPs), especially MMP-1 and MMP-2 (Kligman, 1989; Takema et al., 1994). Skin aging can be influenced by both time (normal aging), as well as environmental factors, but the single most influential factor responsible for accelerated skin aging is believed to be ultraviolet (UV) radiation-induced photodamage (Takema et al., 1994).
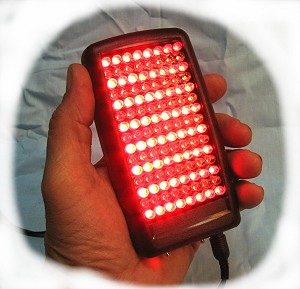
Low-level light therapy (LLLT) is a novel treatment option available for non-thermal and non-ablative skin rejuvenation, which has been shown to be effective for improving skin conditions such as wrinkles and skin laxity (Barolet et al., 2009; Bhat et al., 2005; Dierickx and Anderson, 2005; Russell et al., 2005; Weiss et al., 2004, 2005). A wide range of different light sources have been used to deliver light for these treatments, particularly to the face, and some are shown in Figure 1. LLLT provides increased rates of wound healing, while also reducing post-operative pain, edema and several types of inflammation, making it a highly desirable modality (Calderhead et al., 2008; Kim and Calderhead, 2011). Early studies have reported increases in the production of pro-collagen, collagen, basic fibroblast growth factor (bFGF), and proliferation of fibroblasts, following low-energy laser irradiation in different settings (Abergel et al., 1987; Yu et al., 1994). The use of LLLT sources of wavelengths of 633 nm/830 nm is most common in cases of clinical applications involving wound healing and skin rejuvenation. LLLT is now also used for the treatment of chronic, non-healing wounds via the restoration of imbalances in collagenesis/collagenase, which allows for rapid and enhanced wound healing in general (Kim and Calderhead, 2011).
A study conducted by Lee et al. (2007a) investigated the histological and ultrastructural alterations that followed a series of light treatments, utilizing light emitting diodes (LEDs) with parameters of: 830 nm, 55 mW/cm2, 66 J/ cm2 and 633 nm, 105 mW/ cm2, 126 J/ cm2. Alterations in the levels of MMPs and tissue inhibitors of metalloproteinases (TIMPs) were reported. Increased mRNA levels of interleukin-1 beta (IL-1ß), tumor necrosis factor alpha (TNF-α), intercellular adhesion molecule 1 (ICAM-1), and connexin 43 (Cx43) were also reported following LED phototherapy whereas, IL-6 levels were reported to be decreased. Additionally, a well-marked increase in the amount of collagen was reported in the post-treatment specimens. In fractional-laser resurfacing, the deliberate development of microscopic, photothermally-induced wounds is believed to be responsible for the recruitment of pro-inflammatory cytokines IL-1ß and TNF-α to the site of injury, which contributes to tissue repair. The generation of such a wound healing cascade, thus, contributes to new collagen synthesis.
LLLT for Wound Healing.
LLLT may also, induce wound healing through the non-thermal and non-traumatic induction of a subclinical ‘quasi-wound’, without inflicting thermal injury, and thus, avoiding the complications seen with other therapeutic laser modalities. Additionally, since TIMPs are known to inhibit the activities of MMPs, increased collagen synthesis via the induction of TIMPs, may also contribute to the effects associated with LLLT. Collectively, the findings suggest that an increased production of IL-1ß and TNF-α may be responsible for the stimulation of MMP activity (as an early response to light treatment), which may contribute to the removal of photodamaged collagen fragments, and facilitate new collagen biosynthesis. Furthermore, as a result of therapy, increased concentrations of TIMPs may be observed, which would protect newly synthesized collagen against proteolytic degradation by MMPs. Additionally, the heightened expression of Cx43 may be responsible for enhanced cell-to-cell communication between dermal components (especially, fibroblasts), resulting in greater synchrony between cellular responses, following photobiostimulation (Lee et al., 2007a).
A clinical study by Weiss et al. demonstrated the benefits of LLLT over traditional thermal-based rejuvenation modalities. A group of 300 patients was administered LLLT (590 nm, 0.10 J/cm2) alone, and another group of 600 patients received LLLT in association with a thermal-based photorejuvenation procedure. Of the patients who received solely light treatment, 90% reported an observable softening of skin textures, as well as a reduction in skin coarseness, and fine lines (Weiss et al., 2005b). It was observed that, patients who received some form of LLLT (n = 152) reported a noticeable reduction in post-treatment erythema, and an overall impression of increased efficacy, when compared to the patients that received treatment via a thermal photorejuvenation laser or light source lacking any form of LLLT photomodulation (Kucuk et al., 2010; Weiss et al., 2005b).
LLLT for Acne.
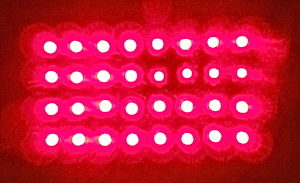
Acne vulgaris is a relatively common skin disorder, with a reported prevalence of up to 90% among adolescents. Phototherapy offers an alternative mode of treatment for acne vulgaris with a suitable profile of side-effects (Rotunda et al., 2004). Sunlight exposure has often been reported to have a significant impact on the treatment of acne, with a high efficacy of up to 70%. More recently, techniques utilizing broad-spectrum visible light (LLLT) are currently being employed for the treatment of acne (Cunliffe and Goulden, 2000). One mechanism of action of phototherapy is via the excitation of porphyrins generated by P. acnes as part of its normal metabolism. These porphyrins act as endogenous photosensitizers, absorbing light (specifically blue light, and to a lesser extent, red light) and stimulating photochemical reactions that generate reactive free radicals and singlet oxygen species, which are toxic for P. acnes (Figure 2) (Lee et al., 2007b; Ross, 2005). Red light has been demonstrated to have a greater penetration depth when compared to that of blue light (Aziz-Jalali et al., 2012). Infrared (IR) light has been proposed to destroy sebaceous glands, and thus, reduce acne lesions (Lloyd and Mirkov, 2002). Red light is believed to stimulate cytokine release from various cells including macrophages, and reduce inflammation (Rotunda et al., 2004; Sadick, 2008).
The sebaceous gland is colonized by bacteria, which can be killed by blue light due to the endogenous porphyrins they produce, acting as photosensitizers and forming reactive oxygen species. Red light can reduce inflammation and stimulate healing with minimal scarring.
Several studies have demonstrated the efficacy of red to near infrared light (NIR) (spectral range 630 nm to 1000 nm, and non-thermal power less than 200 mW) for the treatment of acne vulgaris. Red light may be used alone or in combination with other modalities (in particular, blue light) (Cunliffe and Goulden, 2000; Goldberg and Russell, 2006; Lee et al., 2007b; Posten et al., 2005; Sadick, 2008). One study demonstrated a significant reduction in active acne lesions after 12 sessions of treatment, using 630 nm red spectrum LLLT with a fluence of 12 J/cm2, twice a week for 12 sessions in conjunction with 2% topical clindamycin (Aziz-Jalali et al., 2012). However, the study showed no significant effects when an 890 nm laser was used (Aziz-Jalali et al., 2012). Other studies have reported that the use of blue light and red light in combination, results in synergistic effects for the treatment of acne (Goldberg and Russell, 2006; Lee et al., 2007b; Papageorgiou et al., 2000; Sadick, 2008). It was proposed that the enhanced effects of mixed light were due to synergy between the anti-bacterial and anti-inflammatory effects of blue light and red light respectively (Lee et al., 2007b; Papageorgiou et al., 2000) (Figure 2). In several studies, improvements in inflammatory lesions were reported to be greater than the improvements in comedones (Lee et al., 2007b; Papageorgiou et al., 2000).
LLLT for Herpes Virus.
Herpes simplex virus (HSV) infections are some of the most common types of infections in the present age and are a bane to patients due to the life-long persistence of the virus within the host’s body.
LLLT serves as a suitable alternative to current therapeutic modalities, providing accelerated healing, reduced symptoms, and managing the recurrence of outbreaks (Bello-Silva et al., 2010; de Paula Eduardo et al., 2011; Munoz Sanchez et al., 2012). One study reported that, when LLLT was administered to a group of 50 patients suffering from recurrent perioral HSV infections, during an outbreak-free period (wavelength: 690 nm, intensity: 80 mW/cm2, and dosage: 48 J/cm2), a reduction in the frequency of recurrence of herpes labialis episodes was observed (Schindl & Neumann, 1999). In another study with similar irradiation parameters (intensity: 50 mW/cm2, fluence: 4.5 J/cm2, wavelength: 647 nm), it was reported that intervals of remission were prolonged from 30 days to 73 days in patients with recurrent HSV infections (Landthaler et al., 1983). Intriguingly, the treatment proved more effective in patients suffering from herpes labialis than in those with genital infections. LLLT treatment, however, did not affect established HSV latency in a murine model (Perrin et al., 1997).
The mechanism of action of LLLT in inducing antiviral effects is not known, however, it can be hypothesized that LLLT acts in an indirect manner, influencing cellular and humoral components of the immune system, as opposed to through a mechanism involving direct viral inactivation (Korner et al., 1989). In one particular instance, a study conducted by Inoue et al. investigating suppressed tuberculin reactions in guinea pigs, suggested that the application of LLLT through the use of a low power laser (fluence of 3.6 J/cm2) was responsible for a systemic inhibitory effect on delayed hypersensitivity (Inoue et al., 1989b). Activation and proliferation of lymphocytes (Inoue et al., 1989a; Manteifel et al., 1997; Schindl et al., 1997; Yu et al., 1997) and macrophages (Bolton et al., 1990) as well as the synthesis and expression of cytokines (Funk et al., 1992; Yu et al., 1996) accompanying exposure to low intensities of red and NIR light have been reported on several occasions. Whether or not these findings are actually influential against HSV infection remains to be seen.
LLLT for Vitiligo.
Vitiligo is an acquired pigmentary disorder characterized by depigmentation of the skin and hair. In 1982, a group of investigators looked into the effect of LLLT on the defective biosynthesis of catecholamines (involved in melanin biosynthesis) and discovered that it was able to influence conditions such as vitiligo and scleroderma (Mandel and Dunaeva, 1982; Mandel et al., 1997). Later on, one of the investigators from the same group reported that, following 6-8 months of low-energy HeNe laser (632.8 nm, 25 mW/cm2) therapy there was a noticeable degree of repigmentation in 64% of the patients belonging to a group of 18 individuals, while in another 34% of the patients follicular repigmentation was observed (Mandel et al., 1997). Thus, LLLT has been suggested as a suitable modality for the treatment of vitiligo (Lan et al., 2006, 2009; Yu et al., 2003).
A certain type of vitiligo (called segmental-type) is linked to sympathetic nerve dysfunction in affected areas of the skin and has proved to be resistant to several conventional forms of treatment (Yu et al., 2003). Studies show that LLLT improves nerve injury (Anders et al., 1993; Khullar et al., 1996; Rochkind et al., 1989), and also generates responses to promote repigmentation (Mandel, 1984; Yu, 2000). Thus, the data suggests that LLLT may serve as a potential therapeutic modality for this treatment-resistant form of vitiligo, i.e., segmental-type vitiligo. Upon local administration of a low-powered HeNe laser (3 J/cm2, 1.0 mW, 632.8 nm), it was observed that 60% of the patients showed noticeable perilesional and perifollicular repigmentation with successive treatments. In the same study, upon irradiation of keratinocytes and fibroblasts with a HeNe laser (0.5-1.5 J/cm2), significant increases in the amount of NGF released from keratinocytes were observed. Significant increases in bFGF release from keratinocytes and fibroblasts have also been reported (Lan et al., 2006). NGF and bFGF are known to stimulate the migration of melanocytes, and may contribute to the repigmentation of the process of vitiligo (Peacocke et al., 1988; Wu et al., 2006; Yu et al., 2012). Furthermore, the medium that had been irradiated with the HeNe laser (along with the keratinocytes) led to the stimulation of deoxythymidine uptake and proliferation of cultured melanocytes. Finally, enhanced melanocyte migration was observed, which is thought to have arisen either from the direct action of the HeNe laser or indirectly due to some effect induced by the laser-irradiated medium.
Another study showed that LLLT could lead to enhanced expression of α2β1 integrins, and stimulate melanocyte proliferation (Lan et al., 2009). Also, LLLT demonstrated the ability to induce melanocyte growth through up-regulated expression of phosphorylated cyclic-AMP response element binding protein (CREB), an important melanocyte growth regulator (Lan et al., 2009). Components of the ECM also operate as regulators of factors such as morphology, migration, tyrosinase activity and proliferation of pigment cells, and thus, are important to the pigmentation process (Hedley et al., 1997; Ma et al., 2006; Morelli et al., 1993). Type IV collagen is an ECM component present in the basement membranes of tissues and is known to have intricate associations with melanocytes in the epidermis, such as promoting melanocyte mobility (Lan et al., 2006). LLLT has been shown to greatly promote melanocyte attachment to type IV collagen, and thus, modulate the physiological functioning of melanocytes (Lan et al., 2009). Fibronectin, among other ECM elements, has been shown to have significant effects on differentiation, and the migration of cultured melanoblasts and melanocytes (Ideta et al., 2002; Takano et al., 2002). An in vivo study conducted by Gibson et al. (1983) demonstrated that the physical distribution of fibronectin was closely associated with the migration path undertaken by melanoblasts during the repigmentation process of vitiligo (Gibson et al., 1983). A significant decrease in fibronectin binding was displayed by immature melanoblast cell lines (NCCmelb4) while a more differentiated melanoblast cell line (NCCmelan5) showed an increase in attachment to fibronectin by about 20% following LLLT (1 J/cm2, 10 mW HeNe laser) (Lan et al., 2006). Lastly, the expression of integrin α5β1 on NCCmelb4 cells was observed to be enhanced, which is responsible for regulation of locomotion of pigmented cells (Lan et al., 2006).
LLLT for Reduction of Pigmented Lesions.
Several studies, especially for vitiligo, show that LLLT exhibits stimulatory effects on pigmentation. Despite these studies, which are supportive of the pigmentation promoting abilities of LLLT, one study showed that, the effects of blue light (415 + 5 nm, irradiance 40 mW/cm2, 48 J/cm2) and red light (633 + 6 nm, 80 mW/cm2, 96 J/cm2) in combination, yielded results where an overall decrease in melanin was observed (Lee et al., 2007b). Melanin levels increased by 6.7 arbitrary units in individuals after blue light irradiation, without a statistical significance (P-value > 0.1), whereas, they decreased by 15.5 arbitrary units, with a statistical significance (P-value < 0.005), following red light irradiation. These findings may be associated with the ability of the laser to brighten the skin tone of the irradiated area, which was reported by 14 out of 24 subjects after the treatment period. Up to now however, no other studies have shown similar results. Considering the differences in parameters used for vitiligo and acne treatments, different effects of LLLT on the same tissue could be attributed to the biphasic dose response of LLLT (Huang et al., 2009).
LLLT for Treatment of Hypertrophic Scars and Keloids.
Hypertrophic scars and keloids are benign fibrotic skin lesions that usually arise following surgery, trauma or acne, and are difficult to remove. Fibroblastic proliferation and excess collagen deposition are the main characteristics of these lesions (Uitto and Kouba, 2000), and, imbalances between rates of collagen biosynthesis and degradation, superimposed on the individual’s genetic predisposition have been implicated in the pathogenesis of keloids and hypertrophic scars. A broad range of surgical (e.g., cryotherapy and excision), non-surgical (e.g., pharmacological administration, mechanical pressure and silicone gel dressings), and laser-based therapies (CO2, pulsed dye, fractional ablative and non-ablative lasers) have been tested with variable success, however, the optimal method of treating these lesions remains undefined (Bouzari et al., 2007; Louw, 2007; Wolfram et al., 2009). Recently, it has been suggested that poor regulation of the transforming growth factor beta-I (TGF-βI) expression and interleukin 6 (IL-6) signaling pathways has a significant role in this process, and thus, the inhibition of the IL-6 pathway and/or TGF-βI expression could serve as a potential therapeutic target (Bouzari et al., 2007; Ghazizadeh et al., 2007; Liu et al., 2004; Uitto, 2007; Wolfram et al., 2009). Reports indicating the effects of LLLT on the reduction of IL-6 mRNA levels (Lee et al., 2007a), modulation of platelet-derived growth factor (PDGF), TGF-β, interleukins such as IL-13, IL- 15, and MMPs, all of which are associated with abnormal wound repair (Barolet and Boucher, 2010; Hamblin and Demidova, 2006), have led to the proposal of LLLT as an alternative to the currently available therapeutic options.
A new promising treatment modality seems to be the utilization of pulsed dye lasers (PDL) of wavelength 585 nm, and is believed to act through the induction of capillary destruction and alteration of local collagen formation (Gauglitz, 2013). Moreover, PDL appears to stimulate the up-regulation of MMPs, which also helps to improve keloids and hypertrophic scars (Gauglitz, 2013). Recommended protocols call for non-overlapping pulse doses of fluences between 6.0 to 7.5 J/cm2 for 7 mm spots, and 4.5 to 5.5 J/cm2 for 10 mm spot; however, results definitively indicating the efficacy of PDL for clinical use are lacking (Gauglitz, 2013). PDL treatments can present with mild side-effects, generally purpura; however, in certain instances reactivation of the keloids has been observed (Gauglitz, 2013). Also in some cases, prolonged hyperpigmentation is observed, particularly, in the case of individuals possessing darker pigmented skin, but can be managed using low fluences.
It is worth mentioning that the 1064 nm Nd:YAG laser has been suggested as a means for improving hypertrophic scars and keloids as the Nd:YAG laser has a greater penetration depth than PDL, and would allow for treatment of thicker scars, but may be limited by decreased efficacy associated with increased penetration depth (Gauglitz, 2013). The use of LLLT as a prophylactic means in order to avoid and impair the formation of hypertrophic scars or keloids has been investigated by Barolet and Boucher (2010). They examined three different cases, wherein a single scar was treated by the patient at home on a daily basis with NIR-LED (805 nm at 30 mW/cm2, 27 J/cm2), following scar revision by surgery or CO2 laser ablation on bilateral areas (Barolet & Boucher, 2010). The first patient had pre-auricular, linear, bilateral keloids, and a post-face-lift procedure, and surgical scar revision/excision had been conducted. The second patient had post-acne, bilateral hypertrophic scars on the chest, and CO2 laser resurfacing had been performed. For the third patient, CO2 laser resurfacing had also been used for post-excision, bilateral hypertrophic scars on the back (Barolet & Boucher, 2010). Collectively, in these studies, it was observed that, the NIR-LED treated scars showed significant improvement over the control scars in all measures of efficacy. Additionally, no adverse effects associated with treatment were reported (Barolet & Boucher, 2010).
LLLT for Healing Burns. In a clinical study by Weiss et al. (2005b) 10 patients were treated with LLLT (590 nm, 0.10 J/cm2), for acute sunburn, once or twice a day for 3 days, where only half of the affected area was treated. A reduction in redness, swelling, burning and peeling was reported by the patients post-treatment. In one of the individuals who received treatment twice a day for 3 days, immunofluorescence staining showed that the LLLT treated area exhibited a reduction in MMP-1. Furthermore, the light treated area also exhibited a decrease in MMP-1 gene activity, both 4 and 24 hours post-UV injury, as shown by reverse transcription-polymerase chain reaction (RT-PCR). Four days after UV exposure, changes in inflammation and the dermal matrix were also reported to be associated with LLLT treatment (Weiss et al., 2005b).
Burns associated with laser treatments themselves are also an issue for patients, as these burns cause great discomfort to the patients. Studies support that LLLT facilitates faster healing. In one study, a group of patients (n = 9) that had received second-degree burns as a result of non-ablative laser therapy, were administered LLLT daily for a week. According to patient and clinician reports, healing of the burns was observed to be substantially faster (50% faster) in patients who received LLLT treatment, over those who did not (Weiss et al., 2005b). In another study, by Weiss et al. (2005b), intentional injury was afflicted on the forearm of a patient, and a CO2 laser and a computerized pattern generator were used to induce two identical burns on the patient’s forearm; one on each side of the forearm. Both sites of injury were given daily dressing changes using a non-stick dressing and Polysporin® ointment, and one of the sites was also treated with LLLT. The injury site that was administered LLLT, displayed accelerated tissue reepithelialization, in comparison to the untreated site.
In a study conducted by Schlager et al. (2000), the efficacy of a low-powered laser (670 nm, 250 mW, 2 J/cm2) was studied using a rat model (n = 30 rats). The rats received burns on their left and right flanks, and one of the burn sites received light treatment, whereas, the other site was left untreated. Macroscopic and histological evaluations of the wounded tissue were conducted, but they failed to show any accelerated wound healing in the light treated areas in comparison to the control wounds.
A study conducted by Ezzati et al. (2009) also tested the efficacy of LLLT for healing burns. The study used a mouse model, where a sample size of 74 mice was used, and each mouse received two, third-degree burns; one proximal (control) and one distal (experimental). The mice were divided into 4 different groups. The mice in the first group received sham-LLLT on the distal burn with the laser powered-off, and were used as the placebo group. Mice of the second and third groups were administered a 3000 Hz-pulsed IR diode laser at the distal burn with fluences of 2.3 J/cm2 and 11.7 J/cm2, respectively. The fourth and final group was treated with 0.2 % nitrofurazone alone. Assessment of the LLLT treated groups, showed a substantial reduction in the incidence of pathogenic infections by microbes such as Staphylococcus epidermidis, Lactobacillus, and Corynebacterium diphtheriae when compared to the baseline. Additionally, the LLLT treated groups showed enhanced tissue healing over the baseline, and nitrofurazone treatment groups. Enhanced healing was reported for the laser with a fluence of 2.3 J/cm2, but it was mostly during the early stages of healing. The most substantial increases in tissue repair were reported for the group that was treated with a fluence of 11.7 J/cm2. Studies suggest that LLLT is able to effectively stimulate tissue repair, by modulating cellular interactions that are responsible for repair. LLLT can induce the release of growth factors by stimulation of macrophages and mast cells. Fibroblast, endothelial cell, and keratinocyte proliferation, which are maintained during adverse situations, can also be stimulated by means of LLLT (Ezzati et al., 2009).
Burn scars are problematic to treat as they progressively worsen with hypertrophy and contracture, thus, with limited treatment options, LLLT may be a potential mode of treatment. In a study consisting of 19 patients with burn scars, the patients were treated with a low-powered light source (400 mW, 670 nm, 4 J/cm2), twice a week over a period of 8 weeks. Post-treatment, the scars were reported to be softer and more pliable. Additionally, relief from pain and pruritus, and, occasional improvements in scar patterns (within mesh grafts) were also reported. These effects were sometimes limited, and thus, complete scar disappearances could not be expected. Moreover, it is important to note that, following treatment, better results were obtained in the cases where the burn scars were not more than 12 months of age (Gaida et al., 2004).
LLLT for Psoriasis. Psoriasis is a chronic and recurrent inflammatory skin condition that affects about 1 to 3% of the population (Gelfand et al., 2005; Stern et al., 2004). Its etiology is not entirely known, however, psoriasis is known to result from the interactions of systemic, genetic, immunological, and environmental factors (Zhang, 2012). Psoriasis patients present with well-demarcated plaques, formed as a result of keratinocyte hyperproliferation, mediated by T-lymphocytes that attack the skin (Griffiths and Barker, 2007).
The regions of the body that are most commonly affected in psoriasis include the knees, elbows, scalp, nails and lower back (sacrum), however, the body in its entirety may be affected. The severity of the condition is measured by assessing the total body area involved in the disease (plaque severity). The different variants of psoriasis include, chronic plaque psoriasis (psoriasis vulgaris) (Griffiths and Barker, 2007), flexural psoriasis (inverse psoriasis) (Laws and Young, 2010; van de Kerkhof et al., 2007), guttate psoriasis (Krishnamurthy et al., 2010), erythrodermic psoriasis (Laws and Young, 2010), palmar-plantar psoriasis, facial psoriasis, and scalp psoriasis, and, almost all the variants result in great morbidity and diminished quality of life for the patient (Finlay et al., 1990). Some of the therapeutic modalities, implemented for the treatment of psoriasis, include topical agent use, systemic drug administration, photodynamic therapy (PDT), UV phototherapy, and laser therapy. Psoralen combined with UVA and UVB phototherapy provided a revolutionary means for the treatment of psoriasis, when it was initially introduced. However, some later studies suggested that, repeated and excess exposure to UVB radiation put individuals at an increased risk of developing skin cancer. Thus, Psoralen + UVA (PUVA) was introduced as a therapeutic modality, with a reduced risk of developing cancer, but its use was still restricted as it did not completely eliminate the risk of cancer. Studies investigating the use of LLLT for treatment, with CO2ablative laser (Bekassy and Astedt, 1985), helium-neon lasers (Colver et al., 1984), and red light photodynamic therapy can be dated to the 1980s (Berns et al., 1984).
Laser treatment provides a variety of advantages over conventional treatment modalities; it allows for selective treatment of a lesion without affecting the surrounding skin, with limited or no systemic effects. It can also be used in combination with other therapeutic modalities, allowing for more effective treatment of resistant lesions. Several studies were conducted using a selective excimer laser of 308 nm wavelength (Asawanonda et al., 2000; Gattu et al., 2009; Trehan and Taylor, 2002). Laser therapy displayed results analogous to those observed in UVB treatment. The laser treatment was effective in that it prevented epidermal cell replication while also suppressing the localized immune responses and thereby reducing the characteristic inflammation observed in psoriasis (Railan and Alster, 2008). However, uncertainty exists regarding the carcinogenic ability of long-term excimer laser exposure. Thus, pulse dye laser (PDL) possessing a wavelength of 585 nm was suggested as an alternative. PDL lasers are commonly used for the treatment of vascular disorders, and thus, have proven to be a legitimate treatment modality for psoriasis due to, the association of increased vascularity with psoriasis (De Leeuw et al., 2009; Ilknur et al., 2006). Furthermore, a recent study which investigated the efficacy of combination 830 nm (NIR) and 630 nm (visible red light) LLLT, for the treatment of recalcitrant psoriasis, has facilitated the consideration of LLLT for the treatment of plaques associated with psoriasis. In the study, patients that presented with psoriasis resistant to conventional treatment were administered sequential treatments with 830 nm and 630 nm wavelengths for two, 20-minute sessions, spaced 48 hours apart for a total of 4 or 5 weeks. The results from the study did not display any adverse effects; rather, the results demonstrated resolution of psoriasis (Ablon, 2010). Although the study was promising, it was limited by its small sample size; however, the results of the study provided motivation for future investigations to look at the applications of LLLT as a therapeutic modality.
LLLT for Treatment of Hair Loss
Hair is amongst the fastest growing tissues of the body, undergoing repetitive and regenerative cyclical changes, with each cycle consisting of telogen (resting), anagen (active) and catagen (physiological involution) stages (Paus and Foitzik, 2004) (Figure 3). During the transition from telogen to anagen, there is stringent regulation of the activation of epithelial bulge stem cells, while transit amplifying (TA) progeny cells arise from the secondary hair germ cells (Tiede et al., 2007). Along the period of the anagen phase, the TA cells display resilient proliferation within the epithelial matrix of the hair follicle. As a result, the end product of the hair cycle (i.e., the bulk of the hair filament) is formed through terminal differentiation of the proliferating trichocytes. The prime regulatory element of progenitor cell activation, hair matrix cell proliferation, and terminal differentiation of trichocytes is believed to be the dermal papilla of the hair follicle (Plikus et al., 2006). The anagen stage represents the growth stage of the hair cycle, and may last 2 to 6 years. The catagen stage, which generally lasts 1 to 2 weeks, is when transitioning of club hair is observed; as it progresses towards the skin pore, and the dermal papilla begins to separate from the hair follicle. The telogen stage which lasts from 5 to 6 weeks, exhibits a complete dermal papillary separation from the hair follicle. Lastly, the cycle progresses again towards the anagen stage as the dermal papilla joins up with the hair follicle and the hair matrix starts synthesizing new hair.
Androgenetic alopecia (AGA) is the most common form of hair loss in men, affecting almost 50% of the male population (Otberg et al., 2007). As the name suggests, AGA refers to hair loss induced in genetically susceptible individuals due to the effects of androgens such as testosterone. Testosterone is a lipophilic hormone that diffuses across the cell membrane to carry out its function. It is converted to a more active form called dihydrotestosterone (DHT), which is responsible for many of the effects observed in AGA. The enzyme responsible for the conversion of testosterone to DHT is 5α-reductase. Two types of 5α-reductase enzymes are found in body tissues: Type 1, which is prevalent in keratinocytes, fibroblasts, sweat glands, and sebocytes, and Type 2, found in skin and the inner root sheath of hair follicles. DHT acts by binding to its nuclear androgen receptor, which is responsible for regulating associated gene expression (Ghanaat, 2010).
Abnormal androgen signaling is responsible for the disruption of epithelial progenitor cell activation and TA cell proliferation, which forms the essential pathophysiological basis for AGA (Itami and Inui, 2005). The exact genes associated with the process of hair loss are not entirely known, however, some genes implicated in hair growth are known, and include genes for desmoglein, activin, epidermal growth factor (EGF), fibroblast growth factor (FGF), lymphoid-enhancer factor-1 (LEF-1), and sonic hedgehog (Ghanaat, 2010). Presently, amongst the treatment options available, the most commonly used include minoxidil, finasteride, or surgical hair transplantation (Otberg et al., 2007). Recently, the United States Food and Drug Administration (FDA) has approved the use of LLLT as a novel treatment modality for hair loss (Wikramanayake et al., 2012) (Figure 4).
Several other forms of hair loss also exist such as telogen effluvium (TE), alopecia areata (AA), and alopecia induced via chemotherapy. AA is an autoimmune inflammatory condition that presents with non-scarring alopecia, where histologic characterizations display intra- or peri-follicular lymphocytic infiltrates composed of CD4+ and CD8+ T-cells (Wikramanayake et al., 2012). AA has two variants, with one being alopecia totalis (complete loss of scalp hair), and the other being alopecia universalis (total loss of body and scalp hair) (Wasserman et al., 2007). The most common forms of treatments for alopecia involve intra-lesional corticosteroids, however, other treatment modalities are also available such as topical and systemic corticosteroids, e.g., minoxidil (used in moderate cases) and anthralin. Contact sensitizers are used when more than half of the scalp is affected. PUVA treatment, cyclosporine, tacrolimus, and biologics such as alefacept, efalizumab, etanercept, infliximab, and adalimumab are also utilized for the treatment of hair loss (Ghanaat, 2010). TE is a condition where abnormal hair cycling results in excessive loss of telogen hair (Ghanaat, 2010). Some of the common causes that result in TE include acute severe illness, surgery, iron deficiency anemia, thyroid disease, malnutrition, chronic illness, and medications (e.g., contraceptives, lithium and cimetidine). Chemotherapy functions by acting on fast-growing cancer cells and destroying them, but it also results in the destruction of fast-growing somatic cells in the body, such as those of the hair follicles, and thus, results in the induction of alopecia. It is usually observed within 1 to 3 weeks of initiating therapy, where the most profound effects are observed (Trueb, 2009).
Quite recently, lasers have gathered much attention due to their remarkable ability to cause selective hair removal, however, in some instances it has been observed that, lasers can result in undesirable effects on hair growth such as increased hair density, increased color or coarseness, or a combination of these (Moreno-Arias et al., 2002a, 2002b; Vlachos and Kontoes, 2002; Wikramanayake et al., 2012). This phenomenon is known as “Paradoxical Hypertrichosis”, and its incidence varies from 0.6% to 10% (Wikramanayake et al., 2012). It has also been reported that low-powered laser irradiation of small vellus hairs, can cause them to transform into larger terminal hairs (terminalization of vellus hair follicles) (Bernstein, 2005; Bouzari and Firooz, 2006). The idea that lasers are able to induce hair growth is not something new. In the late 1960s, Endre Mester, a Hungarian scientist, conducted a series of experiments to investigate the ability of the newly developed lasers to cause cancer in mice, using a low-powered ruby laser (694 nm). The laser exposure failed to cause cancer in shaved mice, but it enhanced hair growth (Mester et al., 1968). This fortuitous observation was the first example of “photobiostimulation” using LLLT, and it opened up a new avenue for the field of medicine (Barolet and Boucher, 2008).
Different mechanisms have been proposed in an attempt to explain the effects of LLLT. In one particular study, this ability of lasers (to promote hair growth) was attributed to a side-effect of polycystic ovarian syndrome (PCOS) present in 5 out of 49 females undergoing IPL laser treatment for facial hirsutism (Moreno-Arias et al., 2002a). Another study suggested that, although lasers were responsible for heat generating effects in tissues, the heat produced was not sufficient enough to induce hair follicle thermolysis, however, it may be sufficient to stimulate follicular stem cell proliferation and differentiation by increasing levels of heat shock proteins (HSPs) such as HSP27, which influence the regulation of cell growth and differentiation (Wikramanayake et al., 2012). Some form of sub-therapeutic injury could potentially cause the release of certain factors that could induce follicular angiogenesis, and influence the cycling of cells (Bouzari and Firooz, 2006).
In 2007, the FDA approved LLLT as a possible treatment modality for hair loss (Wikramanayake et al., 2012). Some of the devices that are used for LLLT in hair regrowth are shown in Figure 4. It is believed that LLLT can stimulate re-entry of telogen hair follicles into the anagen stage, bring about greater rates of proliferation in active anagen follicles, prevent development of premature catagen stage, and extend the duration of the anagen phase (Leavitt et al., 2009; Wikramanayake et al., 2012). Although the exact underlying mechanism regarding how LLLT promotes hair growth is not known, several hypotheses have been proposed. Current data suggests that, the action of LLLT on mitochondria leads to increased adenosine triphosphate (ATP) production, modulation of reactive oxygen species (ROS), and stimulation of transcription factors. These transcription factors, in turn, are responsible for the synthesis of proteins that cause certain down-stream responses leading to enhanced proliferation and migration of cells, modulation of cytokine levels, growth factors and mediators of inflammation, and increased tissue oxygenation (Chung et al., 2012).
In one study, the backs of Sprague Dawley rats were irradiated using a linearly polarized IR laser, and, an up-regulation of hepatocyte growth factor (HGF) and HGF activator was observed (Miura et al., 1999). Another study reported increases in temperature of the skin as well as improved blood flow around areas of the stellate ganglion, following LLLT (Wajima et al., 1996).
Minoxidil is another therapeutic modality available for the treatment of hair loss, however, the exact mechanism of action of minoxidil is not completely understood, but it is known that minoxidil contains nitric oxide (NO), which is an important cellular signaling molecule and vasodilator (Proctor, 1989) that influences a variety of physiological and pathological processes (Hou et al., 1999). Furthermore, NO regulates the opening of ATP-dependent potassium (K+) channels, and thus, is responsible for the hyperpolarization of cell membranes (Rossi et al., 2012). Also, It has been suggested that ATP sensitive K+ channels of the mitochondria, and elevated levels of NO might be involved in the mechanism of action of LLLT (Karu et al., 2005, 2008; Tuby et al., 2006) in areas of the brain and heart (Ignatov et al., 2005; Karu et al., 2004, 2008). Thus, given the dependency of both minoxidil and LLLT on the aforementioned factors, there is possibly some mechanistic overlap between the two modalities.
Other studies have demonstrated that, LLLT is able to modulate 5α-reductase, the enzyme responsible for the conversion of testosterone to DTH, as well as alter the genetic expression of vascular endothelial growth factor (VEGF), which plays an influential role in hair follicle growth, and thus, LLLT is able to stimulate hair growth (Castex-Rizzi et al., 2002; Weiss et al., 2005; Yano et al., 2001). Furthermore, it has been demonstrated that LLLT may stimulate hair growth through the modulation of inflammatory processes and immunological responses (Meneguzzo et al., 2012). A study conducted on C3H/HeJ AA mice models supported this assumption, where the mice were exposed to a LaserComb®, and it was observed that, treatment led to an increase in the quantity of hair follicles, where the majority of the follicles in anagen phase were seen to have decreased inflammatory infiltrates. Taking into account the disruptive effect that inflammatory infiltrates have on hair follicles, along with the notion that several cytokines such as interferon gamma (IFN-γ), IL-1α and β, TNF-α and Fas-antigen, and macrophage migration inhibitory factor, are all involved in cyclical hair growth as well as the pathogenesis of alopecia areata (AA), LLLT may be able to play a significant role in the treatment of AA, due to its modulating effects on inflammation (Wikramanayake et al., 2012).
LLLT for Treatment of Alopecia Areata. A clinical study was carried out to investigate the effect of LLLT on the treatment of AA, consisting of a sample size of 15 patients (6 men, 9 women), utilizing a Super LizerTM; a medical instrument operating on polarized linear light with a high output (1.8 W) of IR radiation (600-1600 nm), possessing sufficient penetration depth to reach deep subcutaneous tissues. The patients received a 3-minute laser treatment on the scalp, either once a week or once every 2 weeks, and were administered additional carpronium chloride 5% twice daily to all lesions. Supplemental oral antihistamines, cepharanthin and glycyrrhizin (extracts of medicinal Chinese herbs) were prescribed as well. The results of the study showed that, 47% of the patients experienced hair growth 1.6 months earlier on areas irradiated with a laser when compared to the areas that were not irradiated (Yamazaki et al., 2003).
In another study, the hair growth stimulating effects of LLLT were studied in a C3H/HeJ mouse model of AA, where the mice were irradiated using a HairMax LaserComb® (the comb emits 9 beams of light at 655 nm, while utilizing the attached combs for parting of hair and allowing for a better delivery of light to the scalp) for 20 seconds daily, three times a week for a total of 6 weeks (Figure 4). When the treatment was concluded, increased hair regrowth was observed in the mice that were treated, but the sham treatment group showed no difference in hair growth. Histological examination of mouse tissues showed that, there was an increase in the content of anagen follicles in the light treated mice, whereas, the sham treatment group exhibited more telogen follicles (Wikramanayake et al., 2012).
LLLT for Treatment of Androgenetic Alopecia. The effects of HeNe laser (632.8 nm) on cyclical hair follicle growth, were studied at doses of 1 and 5 J/cm2 at 24 hour intervals for 5 days, in Swiss albino mice; both with and without the administration of testosterone (Shukla et al., 2010). The mice that received He-Ne laser treatment at a dosage of 1 J/cm2showed greater proportions of hair follicles in the anagen phase, when compared to those of the control group, which received no testosterone or HeNe laser. Furthermore, exposure of the mice to a dose of 5 J/cm2showed a decrease in the proportion of hair follicles in the anagen phase when compared to the control group, which could be due to, the biphasic dose response of LLLT (Chung et al., 2012; Shukla et al., 2010). It was also noted that treatment with testosterone caused an inhibition of hair growth with respect to the control group, which was shown by a significant reduction in the proportion of catagen hair follicles. Despite this finding, mice that were treated with a HeNe laser at 1 J/cm2 and with testosterone still showed an increase in the percentage of anagen stage follicles, when compared to testosterone alone. However, when testosterone treated mice were exposed to a HeNe laser dose of 5 J/cm2; a two-fold increase in the amount of anagen stage hair follicles was observed. These results showed that, the hair promoting ability of LLLT (HeNe laser 1 J/cm2) was higher in combination with testosterone, thus, it can be proposed that cells possessing slow rates of growth or undergoing stressful conditions respond better to the stimulatory effects of LLLT.
Another noteworthy finding of the study was that, in the skin irradiated by the HeNe laser (1 J/cm2), some of the anagen follicles possessed a different orientation, and appeared to arise from a greater depth within the skin (Shukla et al., 2010). Such follicles are characteristic of the late anagen phase of the hair growth cycle, and the observation suggests that LLLT may act by prolonging the anagen phase of the hair cycle (Muller-Rover et al., 2001; Philp et al., 2004). Also, in the HeNe (1 J/cm2) irradiated skin that received testosterone treatment, it was observed that the hair follicles originated from the middle of the dermis, and such type of follicles are generally seen during early anagen phase (Shukla et al., 2010). Thus, when considering the above observations, it can be concluded that LLLT is able to stimulate the re-entry of telogen and catagen follicles into anagen phase. In another study, twenty-four male androgenetic alopecia (AGA) patients were evaluated via global photography and phototrichogram using 655 nm red light and 780 nm IR light, once a day for a period of 10 minutes. Following 14 weeks of treatment, significant increases in hair density and anagen were observed; telogen ratios were observed at both the vertex and occiput, with 83% patients reporting that the treatment resulted in satisfactory results (Kim et al., 2007).
A study was performed to investigate the efficacy of LLLT on hair growth and tensile strength involving 28 male and 7 female AGA patients. Each patient was given a 655 nm HairMax LaserComb® to use at home for a period of 6 months, applying it for five to ten minutes per day on alternate days. The results showed improvements in hair growth in all treated areas for both male and female sexes, however, in the case of males the greatest improvements were observed in the vertex area, whereas, for females the best improvements were seen in the temporal areas. All treated areas of both sexes showed an improvement in hair count, but the vertex area showed the greatest improvement in the male patients (Satino and Markou, 2003). In a double-blinded, sham device-controlled, multi-center, randomized 26-week trial, the same device was tested on 110 male AGA patients, where the patients used the device three times a week for fifteen minutes for a total period of 26 weeks. Noticeable increases in the mean terminal density of hair were observed in the treatment group, when compared to the sham treatment group. Also, subjective assessments of the patients over the 26 week period showed significant improvements in overall hair regrowth, a decreased rate of hair loss, thicker feeling hair, improved scalp health and hair shine (Leavitt et al., 2009).
LLLT for Treatment of Chemotherapy-Induced Alopecia.
About 65% of the patients that receive chemotherapy for cancer develop alopecia, which can have detrimental effects on the psychological health of the patient (Trueb, 2009). It has been proposed that LLLT may serve as a treatment modality to stimulate and promote hair growth in cases of chemotherapy-induced alopecia. In one study conducted in a rat model, the animals were administered varying regimens of chemotherapy, in conjunction with LLLT, using a device that possessed the components (laser unit and switch, lacking comb or handle) of the HairMax LaserComb® (Wikramanayake et al., 2012). In all rats that were given laser treatment; hair regrowth occurred at a faster rate when compared to the sham treatment group (Wikramanayake et al., 2012). Additionally, LLLT did not hinder the efficacy of the chemotherapeutic procedures (Wikramanayake et al., 2012).
LLLT for Fat Reduction and Cellulite Treatment
Lipoplasty and Liposuction. Charles Dujarier, a French surgeon, first introduced the concept of lipoplasty (also known as liposuction) in the 1920s. Dujarier attempted to perform body sculpting on the knee of one of his patients, a model, but ultimately the patient developed gangrene, leading to the amputation of her affected limb, thus, the concept of lipoplasty suffered a major setback (Thorek, 1939). In 1974, Fischer reintroduced liposuction, using a novel arrangement of oscillating blades within a cannula to chisel away subcutaneous fat (Fischer, 1990). In 1983, Illouz reported his 5-year experience with a new liposuction technique that could use relatively large cannulas along with suction tubing to safely remove fat from several regions of the body (Illouz, 1983). This technique ushered in the modern era of lipoplasty. Over the following decades, the concept of tumescent liposuction allowed for better results and decreased morbidity associated with liposuction.
LLLT for Fat Reduction and Cellulite Treatment. Neira et al. first demonstrated the use of LLLT as a new means for liposuction, and successfully utilized it with doses that did not produce any detectable increases in tissue temperature or cause any noticeable macroscopic alterations in tissue structure (Neira et al., 2000, 2002). Prior investigations concerned with the effects of LLLT on wound healing, pain relief, and edema prevention helped pave the way for this therapeutic application (Baxter et al., 1991; King, 1989). The development of LLLT as a therapeutic modality to augment liposuction, while avoiding macroscopic tissue alterations, were based on the determination of optimal parameters such as wavelength and power output for use (Oschmann, 2000). Evidence suggests that wavelengths suitable for biomodulation range between 630 and 640 nm (Al-Watban and Zang, 1996; Frohlich, 1968, 1970, 1975; Sroka et al., 1997; van Breugel and Bar, 1992). Several intriguing observations regarding the effects of LLLT on adipocytes were made using a low-level diode laser (635 nm) with a maximal power of 10 mW, with energy values ranging from 1.2 to 3.6 J/cm2 (Neira et al., 2002). Using scanning electron microscopy (SEM) and transmission electron microscopy (TEM) it was demonstrated that, adipocyte plasma membranes exhibited transitory pore formation as a result of the irradiation. It was suggested that this enabled the release of intracellular lipids from the adipocytes, and thus, supplemented liposuction as it was expected to reduce the time taken for the procedure, allowing for the extraction of greater volumes of fat, and reducing the energy expenditure of the surgeon.
Although the findings associated with LLLT gathered much attention and enthusiasm, a study by Brown et al. (2004) put these findings associated with LLLT into question. They cultured human preadipocytes after 60 minutes of irradiation using an LLLT source (635 nm and 1 J/cm2) and did not find any differences in lipid content when compared to non-irradiated cells. Furthermore, the histological examination of human lipoaspirates and lipoaspirates from a porcine model, treated with LLLT for 30 minutes, failed to demonstrate transitory pores in adipocytes when analyzed using SEM (Brown et al., 2004). Additional data raised questions regarding the ability of red light (635 nm) to effectively penetrate below the skin into the sub-dermal tissues (Kolari and Airaksinen, 1993). Since the data reported by Brown et al. (2004), there have been several reports in the literature that have supported the efficacy of LLLT in lipolysis (Caruso-Davis et al., 2011; Mulholland et al., 2011; Nestor et al., 2013).
Mechanism of Action of LLLT for Fat Reduction.
The fat liberating effects of LLLT on adipocytes have been attributed to its ability to induce transitioning micropores, which were visualized with the help of SEM (Figure 6). Furthermore, it was postulated that these pores stimulated the release of intracellular lipids from the adipocytes. Based on this, it was suggested that up to 99% of the fat stored in the adipocytes could be released, and subsequently removed with the help of LLLT (635 nm, 10 mW intensity, 6 minutes irradiation time) (Neira et al., 2002). However, another study demonstrated that cultured adipocytes when treated with LLLT, exhibited a tendency to attain their native cellular conformation following treatment, which was confirmed using a live-dead assay to assess the viability of these adipocytes following irradiation (Caruso-Davis et al., 2011). An increase in ROS following LLLT has been proposed to bring about lipid peroxidation within the cell membranes of adipocytes, and may be responsible for membrane injury, which could present itself as transitory pores (Chen et al., 2011; Geiger et al., 1995; Karu, 2008; Tafur and Mills, 2008). However, when Brown et al. attempted to replicate the Neira group’s findings (Neira et al., 2002), they failed to see any transitory micropores via SEM (Brown et al., 2004). No further SEM studies have documented these pores, but findings have been reported, that indirectly support the transitory micropore formation theory.
Another proposed mechanism that explains the release of intracellular lipids form adipocytes suggests that, the activation of the complement cascade, which is responsible for the induction of adipocyte apoptosis, results in the subsequent release of intracellular lipid components (Caruso-Davis et al., 2011). To test the feasibility of this theory, a group of researchers exposed differentiated human adipocytes to blood plasma, and treated one group of cells to a laser (experimental), while the control group received no laser intervention. No differences were noticed regarding the complement system components in either group, and it was concluded that LLLT did not act through the activation of the complement cascade (Caruso-Davis et al., 2011).
Other evidence suggests that LLLT is capable of inducing an increase in cAMP levels (Karu et al., 1985, 1999). cAMP is responsible for the activation of certain protein kinases, which further activate certain enzymes such as hormone sensitive lipase, which is responsible for the breakdown of triglycerides into fatty acids and glycerol; both of which can traverse the adipocyte membrane and reach the bloodstream (Honnor et al., 1985; Nestor et al., 2012). However, the findings obtained from cell cultures of human adipocytes treated with LLLT (635-680 nm for 10 min), did not exhibit any increases in glycerol and fatty acid levels, suggesting that fat liberation from adipocytes in response to LLLT is not due to the lypolytic breakdown of the adipose tissue. Interestingly enough, as the cellular components were being examined, the presence of triglycerides in the supernatant of extracted samples seemed to support the theory of transient micropore formation in adipocytes (Caruso-Davis et al., 2011). Although these mechanisms have been worked out independently, the mechanism by which triglycerides could traverse the adipocyte lipid membrane remains uncertain.
Following the initial results obtained by Neira et al. (2000), a subsequent study was conducted where adipose tissue samples, extracted from lipectomy samples of patients via the tumescent method, were treated with a 10 mW diode laser (635 nm, total fluence values ranging from 1.2 to 3.6 J/cm2) for a period of 0 to 6 minutes (Neira et al., 2002). It was discovered that, the tumescent method facilitated greater laser penetration and intensity, and allowed for enhanced fat liquefaction (Neira et al., 2002). A similar model was used to test the efficacy of LLLT on lipectomy, where 12 female patients undergoing lipectomy received extraction of both deep and superficial fat, infra-umbilically, using the tumescent method, followed by LLLT. The results showed the synergistic ability of LLLT to effectively work with the tumescent technique for effective fat removal. It was observed that, without laser irradiation the fat tissue remained intact, and the fat cells maintained their original spherical shape. The supplementary effect of the tumescent method on LLLT is hypothesized to be due to, the stimulation of epinephrine-induced cAMP production via adenyl cyclase, and/or, the enhanced penetrative ability and intensity facilitated by the tumescent solution (Neira et al., 2002).
The efficacy of LLLT in combination with vibration therapy, for reduction in local adiposities has also been studied. The study consisted of a total number of 33 patients including both men and women aged 18–64 years, where the patients were divided into groups depending on whether treatment was to take place in the abdomen, and/or the flanks, thighs or buttocks. The parameters for the treatment of localized adiposities were as follows: 6 Hz (Frequency of Oscillating Platform) with LLLT (635 nm) for 10 min, 9 Hz with LLLT (635 nm) for 2 min, 16 Hz with LLLT (635 nm) for 5 min, and, 7 Hz with LLLT (635 nm) for 2 min. These parameters varied depending on the area being treated, but none of the treatments exceeded a total time period of 28 minutes; to maximize patient comfort, and avoid unnecessary exertion. Several means of analysis were employed to gauge the effect of LLLT on fat reduction including histological and echographic evaluation. It was found that the treatment brought about a significant reduction in the median fat by 6.83 cm for the abdomen and flanks, 3.42 cm for thighs, and, 6.16 cm for buttocks. The greatest results were seen with the abdominal/flank regions, whereas, the thighs showed the least response to treatment (Savoia et al., 2013). Thus, studies such as the aforementioned have attempted to describe the mechanistic functioning of LLLT, but the topic still remains somewhat controversial.
LLLT for Treatment of Cellulite.
Cellulite is a condition observed in about 85% of post-pubertal women, posing a major cosmetic concern for such women, where affected individuals display a characteristic “orange peel” dimpling of the skin, most commonly in areas of the thighs and buttocks. The underlying mechanism regarding the pathophysiology of cellulite is still under investigation, but it is suspected that the enlargement of adipocytes, weakening of connective tissue, and decrease in microcirculation are possible triggering factors, helping to initiate the condition (Gold et al., 2011). Several devices and topical treatment agents are available for managing the condition, but are limited by their abilities to generate only temporary effects. Considering the stimulatory effects of LLLT on circulation, collagen formation, and fat reduction; it may provide an alternative to current treatment modalities. In a study conducted with 83 subjects possessing mild to moderate cellulite, administration of a dual-wavelength (650 nm and 915 nm) laser, in combination with a massage device, was carried out to test the efficacy of LLLT on cellulite. The results demonstrated an improvement in cellulite appearance, as well as a 71% reduction in the circumference of patient thighs that were treated; as compared to a 53% reduction in the circumference of the thighs belonging to the control group (Gold et al., 2011).
Topical phosphotidylcholine-based anticellulite gels have also been used, along with LED arrays (660 nm and 950 nm), as an experimental modality for the reduction of cellulite (Sasaki et al., 2007). The results of the study were intriguing as LLLT alone failed to generate improvement in cellulite, but in combination with the topical anti-cellulite gel, LLLT was able to bring about remarkable cellulite reduction (Sasaki et al., 2007). Eight, out of nine, patients were reported to have experienced a reduction in cellulite of the thighs when LLLT was used in combination with the anti-cellulite gel (Sasaki et al., 2007). Further clinical examinations, measurements, and ultrasound evaluations showed a noticeable reduction in hypodermal thickness, and supported the results (Sasaki et al., 2007). However, 18 months following treatment, it was reported that five of the improved thighs had reverted back to their original grade of cellulite, and only three remained with their improved status. Such studies have shown that LLLT can be a promising treatment modality as an alternative to current treatment modalities, especially, when used in combination with other existing modalities. Current literature suggests that, LLLT may have a broad range of applications with a relatively small profile of adverse effects, however, the full extent of its potential remains unknown.
Conclusion
LLLT has been investigated as a novel therapeutic modality for the treatment and management of several dermatological conditions. The majority of the applications of LLLT have been concerned with some form of skin rejuvenation (mostly, the reversal of chronic photodamage). Several studies have demonstrated the use of LLLT for photorejuvenation, photoprotection and the treatment of conditions such as acne and vitiligo. More recent data demonstrates its potential for the treatment of cosmetic conditions such as alopecia, cellulite and adiposities. Furthermore, LLLT is a modality that provides a patient-friendly treatment approach, with its noninvasive mode of action, mild side-effects and convenience of use. LLLT shows promise for future applications, being a novel treatment modality, which not only works well on its own, but also in association with other therapeutic modalities. With growing acceptance and continuing research in the field of photomedicine, it can be concluded that LLLT, among other phototherapeutic modalities, will continue to grow and emerge as a versatile tool in the field of dermatology.



2 Comments to Light Therapy Research